Head injury
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer
|
Aim
To guide Emergency Department (ED) staff with the assessment and management of head injury in children.
Background1
History1
- Time and mechanism of injury
- History surrounding injury e.g. syncope (explore causes), inconsistent history for injury, consider non-accidental injury (NAI)
- Loss of consciousness (LOC) and duration
- Nausea and vomiting
- Trajectory of patient’s clinical course: stable, deteriorating, or improving
- Other injuries sustained
- Amnesia - antegrade or retrograde
- Post-traumatic seizure
- Presence of headache
- Relevant background - ventricular shunt, bleeding tendency / disorder, anti-platelet medications, anti-coagulant medication.
Severe Mechanism of Injury
- Motor vehicle accident (MVA) with patient ejection, rollover or death of another passenger
- Pedestrian or bicyclist without helmet struck by motorised vehicle
- Fall >1 metre in children <2 years; and >1.5m for children ≥2 years
- Head struck by high-impact object (e.g. golf ball, cricket ball).
Examination
- Primary survey and resuscitation
- Head - palpate for depressed skull fracture, boggy swelling
- Pupils - equal, reactive, size
Fundi.
- Papilloedema is not usually seen acutely.
- Retinal haemorrhage in NAI.
- Signs of base of skull fracture:
- Haemotympanum
- Panda eyes
- Battles sign (bruising over mastoid process)
- Cerebrospinal fluid (CSF) leak (ear or nose).
- Signs of raised intracranial pressure (ICP):
- Cushing’s reflex (hypertension and bradycardia)
- Deteriorating Glasgow Coma Scale (GCS)
- Focal neurological signs
- Unilateral/bilateral pupillary dilatation
- Abnormal posturing
- Full neurological examination
- Formal GCS
Risk Factors for Clinically Important Traumatic Brain Injury1
- GCS ≤ 14 or other signs of altered mental status (agitation, drowsiness, repetitive questioning, slow response to verbal communication)
- Severe mechanism of injury
- Post-traumatic seizure(s)
- Abnormal neurological examination
Specific risk factors for children aged less than 2 years:
- Palpable skull fracture
- Occipital or parietal or temporal scalp haematoma
- History of LOC 5 seconds or more
- Not acting normally as per parent
Specific risk factors for children aged 2 years and older:
- Signs of base of skull fracture
- History of LOC
- History of vomiting
- Severe headache
- Isolated vomiting, without any other risk factors, is an uncommon presentation of clinically important traumatic brain injury.
Vomiting, regardless of the number or persistence of vomiting, in association with other risk factors increases concern for clinically important traumatic brain injury.
General Management1
If the child has none of the risk factors above, they are very low risk and there is no need for observation.
If the child has any of the risk factors the recommended observation period is up to 4 hours post injury, including 1 hour return to normal.
Duration of observation may be modified based on patient and family variables.
Frequency of observation to be ½ hourly for the first 2 hours, then 1-hourly until 4 hours post injury. After 4 hours, continue 2-hourly as long as the patient is in hospital.
| No risk factors |
Not intermediate or high risk
AND
Clinically improving
|
≥ 2 Risk factors
OR
Post-traumatic seizure
OR
Persistent headache or persistent vomiting >4 hours post injury
|
Palpable skull fracture
OR
Signs of base of skull fracture
OR
Worsening signs/symptoms
OR
Persistent GCS <14
OR
Persistent altered mental state
|
| Discharge with advice |
Observe for up to 4 hours post injury
Discharge if patient returns to normal for at least 1 hour with advice
|
Senior review to determine need for Computerised Tomography (CT) scan or observation. |
CT scan and inform senior doctor |
Table 1: Risk stratification of Paediatric Head Injury (based on Paediatric Research in Emergency Departments International Collaborative (PREDICT) algorithm: imaging & observation decision-making for children with head injuries)1
If the patient is classified as intermediate risk on the PREDICT algorithm, they require a senior review to determine if imaging is required.
Patients classified as high risk should have imaging and a senior doctor must be informed.
Indication for head CT
The PREDICT algorithm should be used for children with mild to moderate head injuries to assist in our decision to observe, image with a CT scan or discharge.
Children with delayed initial presentation (24-72 hours post injury) and GCS 15 should be risk stratified the same as children presenting within 24 hours.
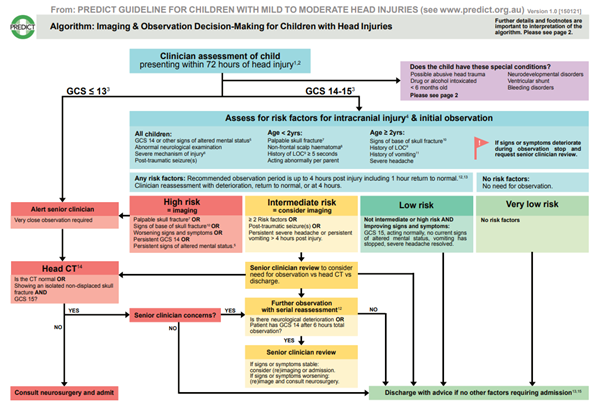
Access the above algorithm as a scalable PDF.
Indications for cervical spine (c-spine) CT
- GCS < 13 on initial examination
- Intubated
- Focal neurological signs
- Paraesthesia on upper limb or lower limb
- Strong clinical suspicion despite normal X-ray
- Plain X-ray difficult to take or inadequate
- Plain X-rays abnormal
- Definitive diagnosis of cervical spine injury needed (e.g., before surgery).
Consider other X-rays and CT as clinically indicated.
Management for Severe Head Injury
The aim is to prevent further secondary injury to the brain after the initial serious primary head injury.
Treatment for:
Hypoxia
- Intubate (continue C-spine precautions)
- Keep end tidal CO2 (ETCO2) 35-40mmHg
- Maintain oxygen saturations at 100%
- Keep head in midline at 30 degrees
- Insert nasogastric tube (orogastric tube if concerned about a base of skull fracture).
- Consider cooling.
Hypotension
- 20mL/kg of sodium chloride 0.9% IV bolus (repeat as required)6
- Consider inotrope infusion.
Raised intracranial pressure
- Sodium chloride 3% (hypertonic saline):
- Mannitol 20% solution
NB: 1g/kg dose is equivalent to 5mL/kg of a 20% solution3
- 1 month – 18 years, IV infusion 0.25–0.5 g/kg over 20–60 minutes; repeat every 2–6 hours if necessary. Higher doses may be required, e.g. 1 g/kg3
- Hyperventilation to decrease End-Tidal Carbon Dioxide (ETCO2): 35-40.
Seizures
- Levetiracetam – loading dose
- Neonates: Refer to Levetiracetam - Neonatal Medication Guideline (internal WA Health only)
- ≥ 4 weeks– 18 years, IV/intraosseous 40 mg/kg (maximum 3 g)4
- Administration:
- Dilute dose to 15mg/mL or less with a compatible fluid and infuse over 15 minutes5
- Status epilepticus in children over 3 months old: dilute dose with an equal volume of sodium chloride 0.9% (to a minimum of 10mL) and infuse over 5 minutes5
- Refer to Seizure - Medication - ED Guideline
Admission criteria
Children who will need admission:
- Severe head injuries.
- Moderate head injuries with:
- Abnormal CT - admit under neurosurgical team.
- Children who have not had a CT and need a period of observation - admit to the ED Short Stay Unit (ESSU)
- Children with normal CT but ongoing concussive symptoms requiring observation - admit to the ESSU.
Special Considerations
- Possible NAI - discuss with senior doctor. Admit and link with General Paediatric team and Child Protection Unit.
- Ventricular shunts - Consider observation over immediate CT scan if there are no risk factors. If there are local signs of shunt disconnection / fracture (e.g. palpable disruption or swelling) or signs of shunt malfunction, consider obtaining a shunt series and consult neurosurgical services.
- Bleeding risk:
- Coagulation factor deficiency: Seek advice from treating haematology team. Decision to CT scan or observe should not delay administration of replacement factor.
- Idiopathic Thrombocytopaenia Purpura (ITP): Check platelet count and blood group in all symptomatic patients (if not already available). For ITP with platelet counts <20x109/L, discuss with haematology and consider steroids or empiric platelet transfusion
- Anti-coagulant or anti-platelet therapy: Consider CT regardless of presence/absence of risk factors for intracranial injury. Discuss with team managing anticoagulation regarding early consideration of reversal agents. Check the appropriate anticoagulant measure (e.g. International Normalised Ratio (INR), Factor Xa inhibitors).
- Neurodevelopmental disorders - These children may be difficult to assess. Consider structured observation or CT scan and include those that know the child best in shared decision making.
- Intoxication - Treat as if neurological findings are due to the head injury. Decision to CT scan or observe should be informed by risk factors for intracranial injury rather than intoxication.
- Less than 6 months of age - consider at higher risk of intracranial injury with lower threshold for observation or imaging. Discuss with a senior doctor.
Nursing care
- Complete and record a full set of observations on the Observation and Response Tool and record additional information on the Clinical Comments chart.
- Complete and record a full set of neurological observations.
- All patients with no Risk Factors must have baseline full neurological observations (FNO) recorded and least hourly visual observations (FNO should be performed if any deterioration or change in condition occurs)
- Children with any of the Risk Factors require observations to be ½ hourly for the first 2 hours, then 1-hourly until 4 hours post injury. After 4 hours, continue 2-hourly as long as the patient is in hospital.
- Cervical spine precautions (if injury mechanism warrants)
- Analgesia if required.
Discharge
All patients who are discharged home should be given the Head Injury - Health Facts sheet which includes ‘Return to Sport’ information.
Post concussive symptoms are common, and advice should be given regarding rest and gradual return to activity. Discuss the Head Injury and Return to Sport Fact Sheet and direct parents to these websites:
References
- Australian and New Zealand Guideline for Mild to Moderate Head Injuries in Children – PREDICT. 2021. Australian and New Zealand Guideline for Mild to Moderate Head Injuries in Children
- PREDICT Algorithm 2021 Cited: 15 February 2022. Available from: PREDICTALGORITHM_v1_1_29.01.21 (2).pdf
- AMH Children’s Dosing Companion (2021) Australian Medicines Handbook Pty Ltd 2021, [Internet] Mannitol; [Modified July 2021, Cited 18 Oct 2021] Available from: Mannitol - AMH Children's Dosing Companion (health.wa.gov.au)
- Levetiracetam [Internet] UptoDate 2022. [Cited 26 May 2022] Available from: Levetiracetam: Pediatric drug information - UpToDate (health.wa.gov.au)
- Australian Injectable Drugs Handbook, SHPA 2022 [Internet] Levetiracetam Cited 15 Mar 2022. Available from Australian Injectable Drugs Handbook,8th Edition
- Advanced Paediatric Life Support: The Practical Approach, Sixth Edition 2015 Wiley & Sons
- Tasker RC, Elevated intracranial pressure (ICP) in children: Management. [Intenet] UpToDate [Last updated April 2022. Cited: 26 May 2022] Available from: Elevated intracranial pressure (ICP) in children: Management - UpToDate (health.wa.gov.au)
| Endorsed by: |
CAHS Drugs and Therapeutics Committee |
Date: |
Jun 2022 |
This document can be made available in alternative formats on request for a person with a disability.