Paraphimosis
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer
|
Aim
To guide PCH Emergency Department staff with the assessment and management of paraphimosis.
Background1
Paraphimosis develops if the foreskin is retracted, and is left retracted for a significant period of time. The tight band caused by the retracted foreskin results in congestion and swelling of the glans, making it difficult for the foreskin to be returned to its normal position. The unreducible paraphimosis in the Emergency department (ED) warrants an urgent surgical review.
Phimosis is circumferential tightening and narrowing of the edge of the foreskin, resulting in a foreskin which is non-retractile or difficult to retract. This may predispose to paraphimosis if the foreskin is retracted, and to balanitis.
Balanitis refers to infection of the foreskin and glans. Paraphimosis can be misdiagnosed as balanitis. It is important to check the position of foreskin in relation to glans and distinguish between balanitis and paraphimosis. Refer to Balanitis - ED Guideline for treatment.
Management
- Most can be gently reduced in the ED
- Unreducible paraphimosis is a surgical emergency
- If you are unfamiliar with the reduction technique seek early surgical advice.
Analgesia and topical anaesthesia
- Important as a paraphimosis can be very painful
- It is useful to gently apply topical 2%lidocaine (lignocaine) 2% gel or lidocaine (lignocaine) 2.5% and prilocaine 2.5% (e.g. EMLA®) cream as soon as the child arrives in emergency, to allow time for topical anaesthesia to occur
- Use of swabs with 20% Mannitol or 50% glucose can be applied to the glans
- A cloth-covered ice pack applied intermittently to the swelling may be a useful adjunct
- The choice of analgesia should be made on assessment of the child's distress and it may be appropriate to use oral oral paracetamol + / - oxycodone, titrated intranasal fentanyl or inhaled nitrous oxide
- One may need to modify the approach to keep the child comfortable and non-distressed
- Refer to Analgesia - ED Guideline for further information.
Technique
- Usually the patient presents early and manual reduction of the foreskin may be attempted in the ED
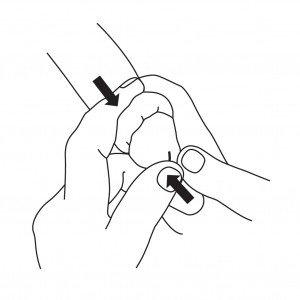
- Following administration of adequate analgesia and sedation, gentle digital circumferential pressure is applied to the swollen glans to reduce oedema
- This process requires patience and may take up to 10 minutes.
- The intention is not to suddenly force the foreskin but to apply constant pressure distal to the foreskin band (greater than arterial pressure), thus slowly shrinking the glans as the oedema settles. This will eventually allow the foreskin to gently slip forward over the glans.
- There is no need to prescribe antibiotics
- Osmotic agents may reduce oedema prior to reduction - use gauze soaked in mannitol 20% or glucose 50%.1
If successful and the patient is able to pass urine normally, he may be discharged with simple analgesia and advised not to retract the foreskin for prolonged periods.
Refer for surgical outpatient review if the patient has a history suggestive of phimosis (as the cause of the paraphimosis).
Failed reduction
- If this fails, or if the patient presents with severe swelling of the glans, the child should be kept fasted and be referred urgently to a paediatric surgeon.
- If the surgical team is unable to reduce in ED, the patient will require emergency theatre to reduce the paraphimosis under general anaesthesia.
References
- Tews M and Singer JI (2020) Paraphimosis Reduction UpToDate. Accessed at www.uptodate.com (external link).
| Endorsed by: |
Nurse Co-Director, Surgical Services |
Date: |
Apr 2022 |
This document can be made available in alternative formats on request for a person with a disability.