Supraventricular tachycardia
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full PCH Emergency Department disclaimer.
|
Aim
To guide staff with the assessment and management of supraventricular tachycardia.
Background
- Supraventricular tachycardia (SVT) is defined as rapid regular, usually narrow (< 0.08 sec) complex tachycardia of 220 to 320 bpm in infants and 150 to 250 bpm in older children
- SVT may be well tolerated in infants for 12 to 24 hours, heart failure later manifests with irritability, poor perfusion, pallor, poor feeding and then rapid deterioration
- Do not use verapamil or beta blockers in infants or children with SVT - can cause profound AV block, negative inotropy and sudden death
- Several atrial rhythms; atrial flutter, atrial fibrillation and sinoatrial node re‐entry tachycardia, are considered subgroups of re‐entrant SVT.
- These do not respond to adenosine but the transient slowing of the ventricular rate may unmask the atrial activity and therefore the underlying cause of the SVT. A running rhythm strip is therefore imperative.
Management
- Assess and manage airway, breathing and circulation.
- A 12 lead electrocardiogram (ECG) in SVT and post conversion is essential.
- Monitoring with a rhythm strip during manoeuvres (i.e. in SVT and post conversion) allows later assessment of underlying rhythm in unclear cases.
- Hypotensive
- Poor peripheral perfusion
- Reduced Glasgow Coma Scale (GCS) score
|
- Seek urgent senior assistance
- Attempt Vagal Manoeuvres (see below) whilst preparing for Direct Current Cardioversion (DCCV)
- Insert IV / Intraosseous needle
- Administer sedation if child is conscious
- Sedation requires a senior doctor (e.g. Emergency Department (ED), Paediatric Critical Care, Anaesthetist)
- Synchronous DC shock.
- 1st shock – 1 Joule/kg
- 2nd shock – 2 Joules/kg
- 3rd shock – 2 Joules/kg
- Consider amiodarone - PCH Medication Manual (WA Health only) in discussion with Cardiologist
|
- Attempt Vagal Manoeuvres
- Infants: ice plus water in bag placed on the face for up to 10 seconds – often effective
- Older children: carotid sinus massage, Valsalva manoeuvre (30 to 60 seconds), deep inspiration/cough/gag reflex, blow into 10mL syringe
|
|
Adenosine IV Rapid Bolus Flowchart for children ≥1 month old
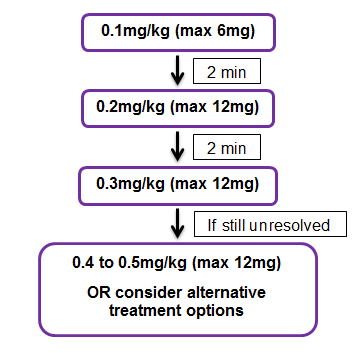
Suggested adenosine dosage adjustment in patients (following discussion with on-call cardiologist):
- Receiving dipyridamole (give 25% of normal dose).
- Receiving the drug via central venous access (give 50% of normal dose).
- With transplanted heart (give 50% of normal dose).
- Hepatic or renal impairment: No adjustment necessary.
[Flow chart and dose adjustment advice taken from the PCH Adenosine Monograph]
|
Administration
Administer via IV site closest to the patient’s heart (therapeutic failure may occur with administration into the lower extremities.
Using a 3-way tap, administer adenosine undiluted over 1-2 seconds, immediately followed by a 10mL sodium chloride 0.9% flush.
Additional information following administration of adenosine
- Monitor blood pressure immediately after the end of a flush.
- Measure blood pressure on the opposite arm to the adenosine infusion to avoid an adenosine bolus effect.1
- If reversion to sinus rhythm occurs but is not sustained, there is little to be gained by repeating the same manoeuvre / drug.
- Discuss with a Cardiologist.
Nursing
Observations
- Record a full set of baseline observations including temperature, pulse rate, respiratory rate, blood pressure and oxygen saturations and record on the Observation and Response Tool.
- 12 lead ECG as soon as possible and have it reviewed by a doctor
- Continuous cardiac monitoring using the defibrillator is preferable as printing and recording an event is instant
- If unwell or unstable – Minimum of 15 minutely pulse rate, respiratory rate, blood pressure and SpO2
- If stable and in sinus rhythm – hourly observations
- Continuous cardiac monitoring for 1 hour post resolution of SVT or longer if specified by medical staff.
Other nursing considerations
- Reassure the child
- Vagal manoeuvres such as ice water on face, Valsalva manoeuvre and carotid body massage will often be attempted after medical review
- If this is unsuccessful then it is likely that the child will require intravenous adenosine.
References
- Burridge N, Collard N, Symons K, Society of Hospital Pharmacists of Australia. Australian injectable drugs handbook. Seventh edition. ed. Collingwood, Vic.: The Society of Hospital Pharmacist of Australia; 2020 [cited. Available from: https://aidh-hcn-com-au.pklibresources.health.wa.gov.au/browse/a/adenosine
| Endorsed by: |
Drug and Therapeutics Committee |
Date: |
Dec 2021 |
This document can be made available in alternative formats on request for a person with a disability.